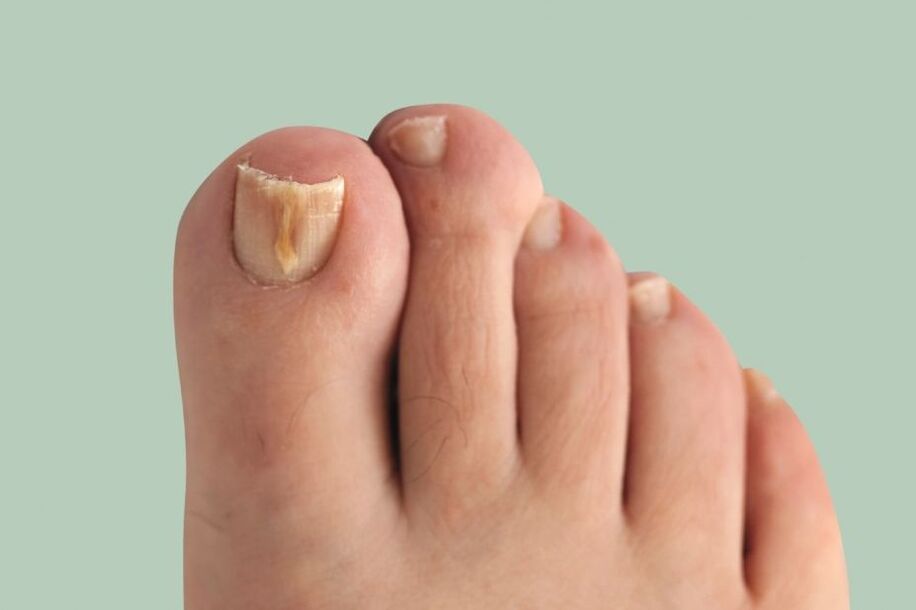
Onychomycosis(nail fungus) is a fungal infection of the nail plate and the structures around it: the nail folds, the matrix (the growing part of the nail) and the nail bed. It manifests itself as deformation and thickening of the nails, a change in their color - the nails become white or yellow.
This disease is quite common. The prevalence of onychomycosis among Europeans, according to some data, reaches 10-12%, exceeding the known indicators of the previous decade. It occurs 1. 5 times more often in men, but they go to the doctor 2 times less often than women. The elderly get sick more often, children very rarely.
The main problem in the treatment of the disease is that patients come to the dermatologist long after the first symptoms appear. Because of this, pathological fungi cover a large area and treatment is delayed.
Pathogenic fungi can only be transmitted by a sick person. Very often, fungal infection occurs within the family, as the source is not identified in time and adequate preventive measures are not taken.
Causes of the disease:the most frequent direct contact with the patient or with the objects he uses (shoes, clothes, bath mats, towels, manicure accessories). Infections often occur when visiting gyms, spas, saunas and swimming pools.
The development of the disease is facilitated by microdamages - cracks in the interdigital folds that occur as a result of abrasion, excessive sweating, dry skin, poor drying after water procedures and flat feet.
Nail mycoses can also occur in the presence of accompanying diseases of the endocrine system (diabetes mellitus, obesity, hypothyroidism), vascular diseases of the extremities (venous insufficiency, lymphostasis), immune disorders, as well as with the use of antibiotics, corticosteroids and cytostatic drugs. As a result of the above diseases, blood microcirculation in the nail area is disrupted and natural immunity decreases, which contributes to the development of secondary infection.
Onychomycosis is caused by the following types of fungi:
- dermatophytes;
- yeast-like fungi of the genus Candida;
- mold fungi.
Depending on the type of pathogen, the penetration of fungal infection and the clinical picture occur differently, so the approaches to therapy also differ.
Toenails are affected by fungus 10 times more often than fingernails. In most cases, fungi are caused by dermatophytes (for example, Trichophyton rubrum). The remaining cases are most often caused by non-dermatophytic fungi (Aspergillus, Scopulariopsis, Fusarium).
If you notice similar symptoms, consult your doctor. Do not self-medicate - it is dangerous for your health!
Along with nail fungus, toenail fungus can also develop. Mycosis of the feet (dermatophytosis, Tinea pedis) is a disease of the skin of the feet, which is caused by pathogenic or opportunistic fungi. Skin changes on the legs are characterized by skin, which is accompanied by itching. In case of severe lesions, on the background of red and swollen skin, erosions and deep cracks appear on the soles and in the spaces between the toes, which are accompanied by pain and make it difficult to walk.
The appearance of modern antifungal drugs has improved the epidemiological situation, but foot mycosis still remains one of the most important problems in dermatovenerology. The use of some drugs is limited to the elderly and patients with chronic diseases.
Routes of infection
The risk of getting infected with fungi is especially high in public places with high humidity. These are saunas, swimming pools, gyms, public baths, etc. The most common routes of infection:
- direct contact with an infected person. Here the fungus moves from its habitat to healthy areas, thus causing an infection;
- domestic way. In this case, the infection occurs when you use the patient's personal items: shoes, personal hygiene items, etc.
Risk factors
The incidence of onychomycosis increases at the age of 60. At this time, the probability of developing such an infection is 60%, which is explained by a slowdown in metabolism, especially in the distal (remote) parts of the body, which are the fingers and toes.
Other risk factors for developing nail fungus include:
- diabetes;
- varicose veins;
- injuries of nails and adjacent tissues;
- HIV and other immunodeficiency conditions;
- long-term use of antibiotics;
- weakened immune system;
- vascular and skin diseases, dermatitis, diaper rash;
- disorders in the blood supply to the extremities;
- insufficient hygiene.
Symptoms of onychomycosis (nail fungus)
The longer the disease lasts, the more pronounced its symptoms become. The main signs of onychomycosis include:
- dyschromia - a change in the color of the nail to yellow, black, green, gray or brown (the type of color depends on the type of fungus);
- onycholysis - separation of the nail plate from the bed;
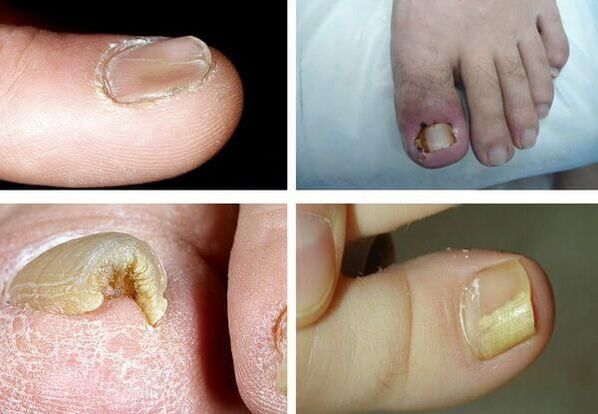
- change in the thickness of the nail plate;
- hapalonychia - a decrease in the thickness of the plaque and its softening;
- koilonychia - the nail looks concave, in the shape of a teaspoon;
- pachyonychia - thickening of the nail plate, nail hypertrophy;
- onychogryphosis - thickening, spotting of the nail plate, curved in the form of a beak;
- change in the thickness of the nail bed (hyperkeratosis - thickening of the nail bed);
- changes in the surface of the nail plate: pits, grooves, ridges;
- changes in the nail folds and surrounding skin (paronychia - inflammation of the proximal nail fold).
It is important to note that none of the symptoms are pathognomonic, d. m. th. , uniquely suitable for a specific pathogen, therefore it is impossible to determine by symptoms - additional examinations are needed.
Pathogenesis of onychomycosis (nail fungus)
The pathogenesis of the disease depends on how the fungus got into the skin and nails.
Distal subungual type:if the fungus has penetrated the skin in the area of the nail folds or in the distal area, then the infection spreads through the free edge of the nail to the bed and further into the matrix. At first, the nail plate may not change, but later, due to hyperkeratosis, it gradually leaves the nail bed and turns yellow. The nail plate can gradually thicken.
White surface type:If white lesions form on the surface of the nail, then over time the fungus takes over the entire nail plate. It thickens, crumbles and takes on a gray-brown shade. In this case, the matrix and epithelium of the nail bed are not affected. There is no inflammation of the surrounding skin.
Proximal subungual type:the fungus can spread from the skin and periungual folds to the nail plate and further into the matrix, reaching the distal parts of the nail plate. Spots appear on the nail in the area of the hole and nail bed, and detachment of the nail plate occurs. There is no significant inflammation of the nail bed or matrix.
Total dystrophic type:The entire nail is affected. The adjacent parts of the nail fold disappear or thicken so that the nail plate can no longer form or grow.
THEREbiophysical concept of onychomycosis pathogenesis, who states that during disease there is a confrontation between two forces: the fungal colony growing towards the matrix and the natural growth of the nail from the matrix at the distal end. Therefore, the speed of nail growth is crucial during the course of onychomycosis - the faster the nail grows, the faster healing will occur. Perhaps this is what explains the low prevalence of the disease in children, since their nails grow faster than those of adults and the elderly.
Classification and stages of development of onychomycosis (nail fungus)
There is the following classification of oncomycosis:
- distal subungual;
- superficial white;
- proximal subungual;
- total dystrophic.

According to the classification of Arievich (1970):
- normotrophic: there are yellow and white lines in the thickness of the nail, but the shape of the nail plate does not change, there is no subungual hyperkeratosis;
- hypertrophic:the nail plate turns yellow, thickens due to subungual hyperkeratosis, becomes brittle, with jagged edges;
- dystrophic:thinning and detachment of the nail plate from the nail bed occurs with the formation of voids.
Complications of onychomycosis (nail fungus)
Long-term onychomycosis increases the risk of developmentdiabetic foot(formation of trophic ulcers on the legs) andgangreneif the patient has diabetes mellitus or vascular disease of the lower extremities.

In immunosuppressive conditions (primary and secondary immunodeficiency), fungi can spread to the skin, internal organs and cause body allergies. This can appear as a skin rash and even the development of bronchial asthma.
In an uncomplicated course, the disease causes traditional symptoms for fungi, causing only severe discomfort to a person. But without treatment, onychomycosis can cause complications. Most often they manifest in addition to a bacterial infection.
Sometimes onychomycosis is very acute with the appearance of blisters, ulcers and weeping areas on the skin near the nail. In severe cases, the disease takes a generalized form. This means that nail fungus spreads to internal organs and systems, and then the patient will require urgent hospitalization.
Diagnosis of onychomycosis (nail fungus)
Before considering the methods for diagnosing onychomycosis, it is necessary to explain how to correctly collect the material for research (the patient does this independently, or prepares the nails before the diagnosis). Before collecting material for research, it is necessary to treat the nail plate with 70% alcohol to avoid contamination with other bacteria.
The method of collecting the material varies depending on the form of onychomycosis:
- surface form- make an itch from the nail plate;
- distal form- both an itch from the nail bed and part of the nail plate are necessary;
- proximal subungual form- the material is collected with a trowel, or a nail biopsy is performed, or scraping from the nail bed.
The fastest method for determining pathological fungi in the nails ismicroscopy. Technique: the material under study is treated with alkali solution to dissolve the keratin. To make the mushroom threads better visible, dye is added to the alkali. The resulting preparation is then studied under a microscope.
This research method is the fastest and most objective. The sensitivity is up to 80%. The disadvantages of the method include the fact that when it is used it is impossible to determine the type of pathogen.
Bacteriological culture: is an additional method for the diagnosis of onychomycosis. The material is planted in a special environment and the result is interpreted under a microscope after 2-3 weeks. This method allows you to determine the type of pathogen - this helps determine treatment tactics and select drugs based on sensitivity. But the disadvantage of the study is that it takes a lot of time, and its sensitivity is only 30-50%.
Biopsy: Using a scalpel and applying anesthesia, the nail and the nail bed are cut. The material is immersed in a formaldehyde solution and sent for histological examination in the laboratory. The advantages of this method are that it is very sensitive and allows you to determine the presence of a pathological fungus in the material.
Disadvantages: it is impossible to identify the pathogen, as well as to determine the viability of microorganisms, the method is expensive and labor intensive.
Gene diagnosis: Molecular biological research (PCR) method. This is one of the new and very sensitive methods for the diagnosis of onychomycosis - it helps to detect the DNA of the causative agent of the disease. In our country, it is recommended to introduce this type of diagnostics in those medical institutions that have PCR laboratories, but at the moment, testing systems for the identification of dermatophytes and mold are only planned to be introduced in laboratories. The method allows you to determine the type of pathogen, and its sensitivity ranges from 80-90%. Disadvantages: high cost, inaccessibility, lack of technology standards and complexity of implementation.
More and more, doctors are putting it into practicedermatoscopy. Using this method, you can evaluate changes in the color and structure of the nail, as well as the condition of the surrounding structures. Dermatoscopic examination allows a more accurate assessment of the depth of damage to the nail plate and a more accurate calculation of the onychomycosis severity index (KIOTOS).
First of all, the patient is sent for microscopy, which allows to identify the presence of the pathogen. In the future, it is necessary to determine its type in order to choose the right treatment for toenail fungus. In JSC "Medicine" (clinic of Academician Roitberg) in the center of Moscow, the most modern and widespread methods for the diagnosis of onychomycosis are practiced:
- cultural examination of a biological sample of the affected tissue. To do this, it is placed in an artificial nutrient medium, where the pathogen grows to determine its type;
- Polymerase chain reaction (PCR) method to detect pathogen DNA in a sample of affected tissue.
When you see a doctor
Many who have encountered onychomycosis know that the disease develops slowly and is extremely difficult to treat. Therefore, it is very important to consult a doctor when the first signs of the disease appear. A dermatologist treats nail onychomycosis in our clinic in the center of Moscow. The specialist will provide you with competent help and guide you to full recovery.
Preparing to visit the doctor
Before visiting a dermatologist, it is important not to treat the affected nail areas with anything, d. m. th. do not use medications, including iodine and brilliant green. It is also necessary to avoid the use of anti-fungal creams and ointments. At your appointment, you should have all the tests taken previously, including those for other diseases. Affected nails should not be cut 3-4 days before the consultation.
Treatment of onychomycosis (nail fungus)
There are several types of treatment for onychomycosis:
- Local therapy.
- Systemic therapy.
- Combined therapy.
- Corrective therapy.
Local therapyinvolves applying medications to the nail plate and nail folds. Indications for local therapy:
- Limited form of damage to the nail plate (according to KYOTO).
- There are contraindications for prescribing systemic drugs: hypersensitivity, liver disease, kidney dysfunction, pregnancy, lactation.
The advantages of this therapy are that high concentrations of the therapeutic agent are formed on the surface of the nail, which does not penetrate into the bloodstream. There are no side effects from the use of antifungal drugs - nausea, loss of appetite, abdominal pain. The disadvantage of the method is that the medicinal substance does not always reach the habitat of the pathogen, especially if the fungus is located in the nail bed or matrix. This in turn can lead to treatment failure. This type of treatment is very troublesome, since before applying the medicine it is necessary to remove the affected part of the nail.
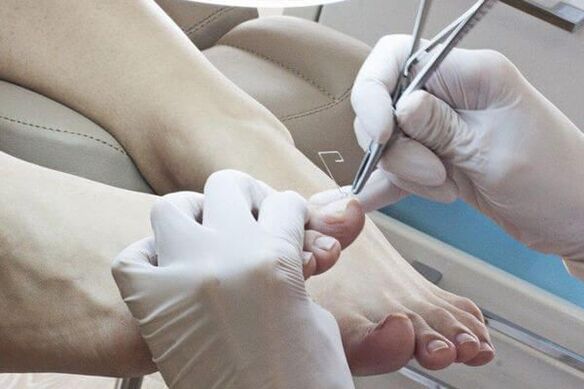
Methods for removing affected nails:
- Mechanical removal using files, suction or a drill.
- Use of keratolytic patches. Before applying the keratolytic plaster, the skin around the nail is closed with a plaster, a plaster mass is placed on top (urea with salicylic acid) and closed with an adhesive plaster. The plaster mass is changed every 2-3 days. After each removal, the affected part of the nail is removed mechanically.
- Surgical. This operation is very painful and traumatic, as with the removal of the nail plate, the growth area can be damaged, which leads to the regrowth of deformed nails.
Local antifungal agents are used after removal of the affected nail plate.antimycoticdiffer according to the place of application:
- applied to the nail: varnish;
- applied on rollers: creams, ointments, solutions.
The most studied drug for topical use isNaftifin solution 1%., which has an evidence base for treatment effectiveness based on a Cochrane meta-analysis. This product is water-based, which facilitates better penetration of the antifungal substance into the affected area. Varnishes, whose active ingredients are ciclopirox and amorolfine, have a dehydrated base, which reduces the penetration of the drug into the deep layers. Therefore, dermatologists consider the use of varnishes unsatisfactory and increasingly prefer water-based products.
To get results from local therapy, it is necessary to follow the treatment regimen, it is important that the patient is responsible, stable and patient. The duration of therapy can be up to 12 months.
Systemic therapyallows the antifungal drug to penetrate the bloodstream at the site of the lesion, even if the nail bed and matrix are affected. A high concentration of the drug remains in the affected area for a long time after the end of use. The disadvantages of this type of treatment are associated with the risk of side effects and toxicity.
Indications for systemic therapy:
- Common forms of damage to the nail plate.
- Lack of effect from local therapy (ie, after six months of treatment for onychomycosis on the hands and 9-12 months of treatment for onychomycosis of the feet, healthy nails did not grow back).
To determine treatment tactics, KIOTOS (Clinical Index for the assessment of the severity of Onychomycosis by Sergeev) is used, proposed by A. Yu. Sergeev in 1999. It is used as a therapeutic standard in different countries of the world.
medicationsfor the treatment of onychomycosis can be classified as follows:
- antimycotics - have an antifungal effect;
- antiseptics - have antifungal and antibacterial effects. They are rarely used, only if there are no other antifungal agents;
- multicomponent - in addition to the antifungal agent, they also contain other drugs, such as anti-inflammatory drugs.
Recipe Modes:
- standard - taking drugs every day during the prescribed period of treatment;
- shortened - the treatment period is shortened, it can be carried out in regular doses or increased;
- intermittent - the treatment is prescribed in several short courses, the intervals between the courses are equal to the duration of the courses;
- pulse therapy - the treatment is prescribed in several short courses, the intervals between the courses are longer than the duration of the courses.
Antifungal drugs are divided according to the active substance:
- triazoles;
- allylamine;
- others (third generation drugs).
It is currently used for systemic therapyonly third generation drugs.
With combined therapylocal and systemic treatment are performed simultaneously. Combined therapy is used when it is necessary to increase the effectiveness of systemic therapy and reduce treatment time.
Corrective therapy(treatment of associated diseases): to choose a treatment regimen, it is necessary to assess the general somatic condition of the body. Diseases such as circulatory disorders in the extremities can reduce the access of the antifungal agent to the lesion. Therefore, drugs that improve tissue trophism have been prescribed.
Due to the toxic effect of systemic antifungal drugs, it is necessary to exclude liver diseases and, if necessary, to prescribe hepatoprotectors.
Home remedies
Before using home remedies, you should consult your doctor. With his permission, you can use the following recipes:
- iodine. Before use, the feet should be steamed, washed with laundry soap, and then the affected areas of the nail plates should be removed. Then, treat the nails and the skin between the fingers with iodine, put them in a soda bath for 20-30 minutes and dry them thoroughly;
- vinegar. For 3 liters of water take 1 tablespoon. apple cider vinegar and add a little potassium permanganate. Soak your feet in the bath for 20-30 minutes, then dry them completely;
- hydrogen peroxide. After you have completely steamed your feet, remove the affected areas of the nail plates. Put cotton soaked in hydrogen peroxide on them, wrap it with a bandage and leave it for half an hour.
Myths and dangerous misconceptions in the treatment of nail fungus
One of the most important and dangerous myths is that nail fungus is not considered a serious disease. In fact, onychomycosis, as it progresses, can lead to serious consequences, including deformation and complete rejection of the nail from the nail bed.
In addition, an infected person poses a daily risk to loved ones, since being near him, they also risk getting sick. That is why it is important to know how to cure nail fungus in time.
Forecast. Preventing
The sooner the patient consults the doctor with signs of fungal nail infection, the sooner the disease can be cured and the nail plate restored. With long-term processes involving the entire nail, the treatment of onychomycosis can be long, but if all recommendations are followed, recovery often occurs. If there are contraindications for systemic therapy, long-term maintenance treatment with local drugs is necessary.

For preventionIt is necessary to observe the rules of personal hygiene and reduce the possibility of re-infection:
- try to wear comfortable and high-quality shoes (to prevent excessive sweating of the feet);
- It is recommended to change socks and tights every day;
- use only individual shoes. For those undergoing treatment for onychomycosis, shoes should be treated at the beginning of treatment, at least once a month throughout the treatment period and after its completion;
- if necessary, use antiperspirant for feet;
- use an individual bag for nail care (scissors, files);
- before and after visiting public places (swimming pool, bath, gym) use external antifungal agents (sprays, creams and pencils);
- identify the source of the fungal infection in the family and treat it at the same time.
It is recommended to periodically carry out antifungal treatment of personal items, shoes, bathtubs, floors and carpets. For these purposes, you can use a 40% solution of acetic acid, a 1% alcoholic solution of chlorhexidine (prescribed by a doctor) and disinfectant solutions. Linen can be boiled in a 1-2% soap-soda solution for 20-30 minutes, ironed at maximum temperature.























